
La scelta del fissatore esterno avviene in base a:
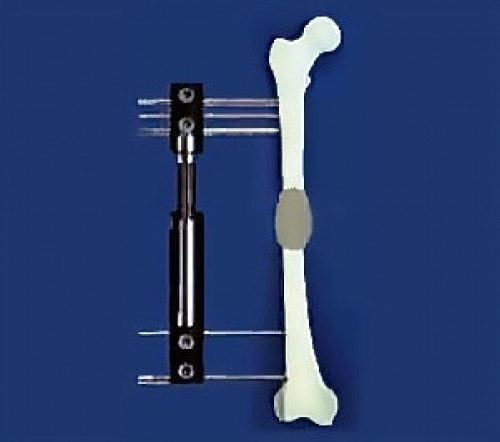
Il fissatore esterno è un apparecchio esterno all’organismo fissato alle ossa per mezzo di perni o viti, attraverso i tessuti molli. Esistono diversi tipi di fissatori esterni : FISSATORI UNILATERALI FISSATORI CIRCOLARI
Sono messi su un lato dell’arto. A livello della coscia, sono posti sulla parte esterna. A livello della gamba, sono posti al suo interno.
Esistono numerosi prodotti: fissatore del tipo Orthofix, Heidelberg, Judet, Wagner, FSA, etc. Le parti esterne (corpo del fissatore), collegate all’osso per mezzo di viti o perni di grosso calibro (4-6 mm), sono ben tollerate dai pazienti.
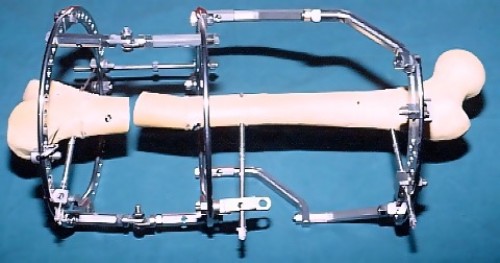
Permettono una migliore stabilità dei frammenti ossei rispetto ai fissatori unilaterali, con l’utilizzo di piccoli perni in tensione (1,5 -2 mm), ma sono meno confortevoli. Permettono correzioni più complesse, ottenute gradualmente nel postoperatorio.
Il primo fissatore è stato progettato da Ilizarov che ha codificato il metodo di allungamento degli arti. Ilizarov ha utilizzato il principio della bicicletta in cui la ruota è tenuta nel centro grazie a perni in tensione, e alleggerendo così il sistema si ottiene una grande stabilità, se rispettati i principi base.
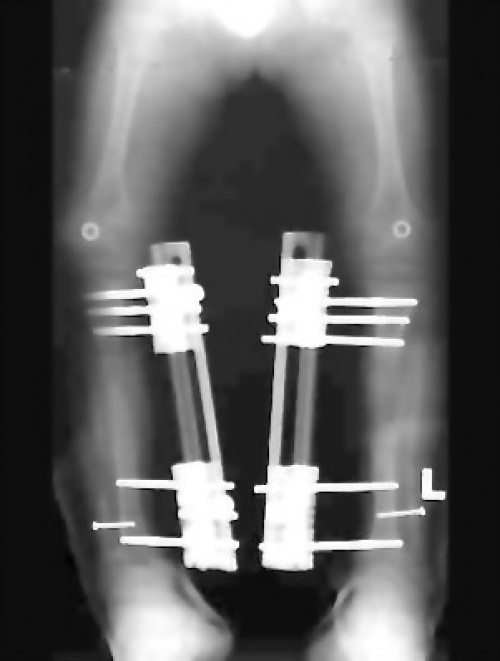
I fissatori esterni, in teoria, possono correggere tutti i piani (e deformazioni) in maniera progressiva. Tuttavia, la complessità di alcune deformazioni, con multiple angolazioni e in parti diversi all’interno dello stesso osso, rendono talvolta la teoria inapplicabile. Per esempio, a livello del piede che è formato da tre parti (avampiede, mesopiede e retropiede), ciascuna con numerose ossa, le deformazioni devono essere corrette separatamente per ogni parte, che a sua volta deve essere corretta nei tre piani dello spazio separatamente. In un secondo momento, deve essere corretta anche la loro relazione in almeno un piano spaziale, determinando così una correzione complessiva nei 3 x 3 + 2 = 11 piani spaziali. Chiaramente è difficile trovare un fissatore esterno provvisto di 11 “cerniere” (o centri di rotazione), che consentano di correggere le deformazioni in tutti i piani spaziali. Inoltre, si selezionano i piani più importanti da correggere. Per le ossa lunghe si possono correggere simultaneamente o sequenzialmente il varismo/valgismo, il flexum/recurvatum, la traslazione, la rotazione, e l’allungamento dell’osso.Tali correzioni possono avvenire progressivamente, ma talvolta, si preferisce realizzare uno o due piani simultaneamente durante l’intervento e riservare la correzione progressiva a uno o due piani addizionali.
ALLUNGAMENTO La distrazione dipende dall’aumento. Generalmente si calcola 1 mm di aumento/giorno. Per 6 cm, si calcolano 2 mesi. Durante questa fase, si può in teoria deambulare sul proprio fissatore esterno, salvo casi particolari. Tuttavia, il fissatore esterno spesso è scomodo e il paziente non deambula normalmente (sbrigare delle commissioni, etc.). La demineralizzazione ossea dimostra l’insufficienza di stimolazione ossea della deambulazione. CORREZIONE PROGRESSIVA (ISOLATA) DEGLI ASSI OSSEI La correzione graduale dura generalmente meno di un mese. In caso di correzione preoperatoria completa fissata da un fissatore esterno, non è necessaria una successiva correzione progressiva.
Generalmente, l’allungamento avviene in diverse fasi :
La fissazione dura circa 1 mese/cm di aumento. In tal modo, per 6 cm, si calcolano 6 mesi di fissazione. I muscoli si distendono e si adattano alla loro nuova lunghezza. Spesso il paziente comincia a deambulare meglio. L’osso si rinforza sufficientemente per consentire l’ablazione del fissatore esterno.
La dinamizzazione è la fase in cui si allentano tutti i dadi affinché le forze, durante l’attività muscolare e la deambulazione, non passino più attraverso il fissatore esterno ma attraverso l’osso. Così facendo, l’osso riceve tutte le forze meccaniche e può rinforzare la sua struttura più facilmente. Per molte equipe, questa fase impiega circa un mese, ma in caso di distrazione a 60-300 volte/giorno, tale fase viene eliminata.
La durata dell’utilizzo del gesso o dell’ortesi è di circa un mese, ma, talvolta, si può evitare questa fase.
Il recupero delle attività è progressivo con ripresa della deambulazione. Generalmente si sconsiglia l’attività sportiva il mese seguente l’ablazione del fissatore, per rischio di frattura del rigenerato osseo. La durata totale per un allungamento di 8 -10 cm è di 10-18 mesi con un fissatore.
Prevede le seguenti fasi :
La fissazione dura generalmente circa 3 mesi in assenza di allungamento osseo, che corrisponde al ritardo del consolidamento di una frattura.
La dinamizzazione spesso precede l’ablazione del fissatore esterno.
Per definizione i fissatori esterni hanno perni/viti che attraversano i tessuti molli e mettono in contatto l’ambiente esterno, considerato sporco, contaminato, con l’ambiente interno pulito, sterile. Portare un fissatore esterno prolungatamente implica un rischio infettivo che si manifesta generalmente intorno ai perni. Per questo motivo sono necessari cure particolari e visite regolari del chirurgo, durante l’allungamento o la correzione. Inizialmente le visite sono settimanali o ogni due settimane, successivamente sono più distanziate nel tempo. Il paziente dovrà proteggersi dai rischi derivati dallo sporco e pulirsi, o farsi dei bagni, in una certa maniera (il metallo utilizzato non si arrugginisce). Ogni giorno dovrà girare i dadi per effettuare la correzione o l’allungamento. In genere, l’aumento è di 1 mm di correzione al giorno ottenuto in quattro volte nella giornata. Le operazioni di allungamento sono generalmente poche o non dolorose. Agendo al di fuori del suo organismo (dadi), il paziente avrà pochi timori e stress psicologici. Tuttavia, lo stiramento dei tessuti molli sui perni/viti del fissatore esterno può causare dolori da moderati a molto moderati. Le cure dei perni devono essere eseguite molto bene per eliminare il rischio di complicazioni sugli stessi.
Le complicazioni possono essere suddivise in gruppi. Sono spesso più gravi negli allungamenti, soprattutto quelli che superano il 15% della lunghezza iniziale dell’osso allungato, e derivano dall’inevitabile ambivalenza dei fissatori esterni: devono essere portati il più a lungo possibile, affinché l’osso diventi molto solido, ma allo stesso tempo, devono essere portati il minor tempo possibile, per evitare il rischio di infezioni. INFEZIONI RIGIDITÀ ARTICOLARE DEVIAZIONI D'ASSE FRATTURE OSTEOPENIA/OSTEOPOROSI LESIONI NERVOSE O VASCOLARI POSTOPERATORIO
Sono le complicazioni più frequenti. Localizzate in genere attorno ai perni, con delle piccole secrezioni, reagiscono bene ai trattamenti locali e agli antibiotici. Raramente richiedono un nuovo intervento per un problema ad un perno.
Per la presenza dei perni, i tessuti molli non possono muoversi facilmente, in tal modo si può riscontrare rigidità o diminuzione della mobilità articolare. In generale la rigidità regredisce lentamente dopo l’ablazione del fissatore esterno, ma talvolta, sono necessari1 o 2 anni per recuperare una normale mobilità articolare.
Controllare l’asse delle ossa, anche se si può agire facilmente sul fissatore esterno, non è facile. Dopo l’ablazione del fissatore, l’osso è ancora in piena attività di costruzione e di rimodellamento quindi più plastico e deformabile. Si riscontrano talvolta deviazioni secondarie per curvamento sull’osso fragile. Fortunatamente, questi gravi problemi necessitano raramente di un nuovo intervento, tuttavia, spesso è necessario un periodo di fissazione in un gesso, dopo l’ablazione del fissatore esterno, affinché l’osso diventi più solido meccanicamente.
Sono rare (circa il 10% o inferiori al 10%), ma giustificano una fissazione temporanea nel gesso dopo l’ablazione del fissatore esterno.
È inevitabile e si manifesta con una decalcificazione visibile alla radiografia: l’osso diventa trasparente. Dopo l’ablazione del fissatore esterno, l’osso riprende una densità di qualità migliore.
I russi dell’Istituto Ilizarov hanno ricavato la quantità totale di calcio dell’organismo negli allungamenti per mezzo di fissatori esterni. La perdita di Calcio è del 10% del contenuto corporeo totale (100 gr). Ciò giustifica un’integrazione calcica e vitaminica (Vit. D) durante tutto l’allungamento.
Le lesioni possono essere dirette (rare, durante l’intervento) o secondarie per stiramento dei tessuti molli. In generale, quando ciò accade, s’interrompe l’allungamento o si raccorcia l’osso allungato, e il recupero avviene progressivamente.
Portare un fissatore esterno può essere stancante almeno all’inizio e per certi pazienti, rappresenta uno “shock” non tanto fisico quanto psicologico: il bambino spesso nasconde l’arto con il fissatore esterno, ma presto, imparerà ad abituarsi. Il trattamento è lungo e il paziente passerà diverse fasi psicologiche. Talvolta, nel bambino si può riscontrare anche una fase depressiva mascherata. A maggior ragione, sono necessari un forte sostegno familiare, senza dar luogo ad infantilismi iperprotettivi, e talvolta anche l’aiuto di uno psicologo. Tutti i trattamenti lunghi (come le leucemie o i tumori) lasciano dei segni nel bambino che possono avere delle conseguenze sul suo vissuto psicologico e ripercuotersi in età adulta. L’aspetto relazionale in età adulta può essere influenzato dai trattamenti che il bambino ha subito.
Weymouth Street Hospital
42-46 Weymouth St.
London W1G 6DR
Princess Grace Hospital
30 Devonshire Street
WYG6PX Londra, UK
+39 0236758514
Harley Street Specialist Hospital
18-22 Queen Anne St.
London W1G 8HU
Studio Dr. Guichet
Corso Magenta, 44
20123 Milano, IT
+39 0236758514